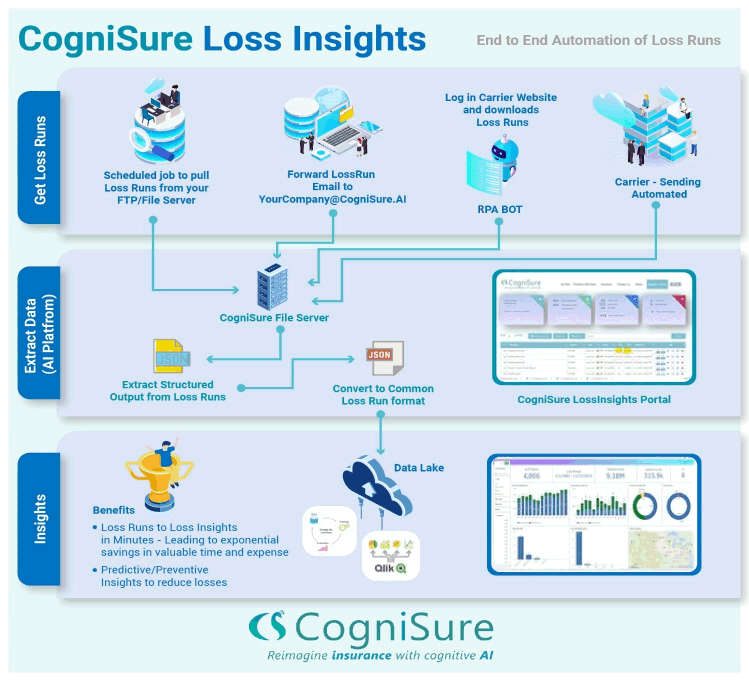
COGNISURE LOSSRUN INSIGHTS AUTOMATES the END to END PROCESS of LOSS RUNS


Loss run processing is a major pain point for insurers, and improving and automating the intake of loss runs is a significant opportunity for growth, reduction of operating costs, and improvement of risk assessment.
Insurers are losing business due to long turnaround times driven by loss run processing, insurers are miscategorizing and improperly pricing risks due to the error prone manual loss run process, and insurers are wasting time and money on every incoming new business and renewal application that can be better spent on higher value tasks.